Abstract
Cytomegalovirus (CMV) and Epstein-Barr virus (EBV) reactivation are two of the most frequent infections affecting patients receiving allogeneic stem cell transplantation (HSCT). Up to 80% of seropositive patients might experience CMV reactivation in absence of prophylaxis, expecially when a seropositive patient receive stem cell graft from seronegative donor. The introduction of Letermovir notably reduced the risk of CMV infection also in high risk patients. EBV is a herpesvirus widely spread in common population with a prevalence of approximatively 80%. As a consequence, many recipient and donor have EBV seropositive status. We would evaluate if a difference occurred in the CMV and EBV incidence after Letermovir introduction, which casually coincided in our center with the transition to a single graft-versus host disease (GvHD) prophylaxis schedule including cyclophosphamide post (Cy-post).
We enrolled patient submitted to allogeneic stem cell transplant in our centre from January 2015 to december 2020. Patients were divided into two groups. The pre-letermovir group (group A, n=230) included patients who had received prophylaxis with ciclosporine A (CSA) plus micophenolic acid (MFA) (N=17) or CSA plus short course methotrexate (MTX) (N=96) or CSA plus MFA plus Cy-post (n=117). In the post-letermovir group (group B, n=135) all patients received the same GvHD prophylaxis with CSA plus MFA plus Cy-post. Sixty-eight of them received letermovir in addition to acyclovir as CMV prophylaxis.
In the group A, CMV infection rate was affected by HLA mismatch (HR 1.70, p=0.003), Cy-post use (HR1.49, p=0.02), anti-thymocyte globulin (ATG) use (HR 0.62, p=0.01), bone marrow or cord blood source (HR 1.46, p=0.03), CMV seropositive recipient (HR 10, p=0.0001) and CMV seronegative donor for a seropositive recipient (HR 2.2, p<0.0001). Multivariate analysis confirmed CMV seropositive recipient (HR 9, p=0.002), CMV seronegative donor for seropositive recipient (HR 1.67, p=0.008) and HLA mismatch (HR 3.58, p=0.006) as independent variables for CMV infection. EBV infection appeared to be affected by underlying disease remission status at transplant (HR 1.64, p=0.01), HLA mismatch (HR 0.42, p<0.0001), GvHD prophylaxis other than Cy-post (HR 2.60, p<0.0001), ATG use (HR 2.60, p<0.0001), unrelated donor (MUD) (HR 2.01, p=0.0005) and aGvHD occurrence (HR 1.62, p=0.01). Multivariate analysis confirmed aGvHD occurrence (HR 1.74, p=0.007) and underlying disease remission at transplant (HR 1.90, p=0.002) as independent variables for EBV infection.
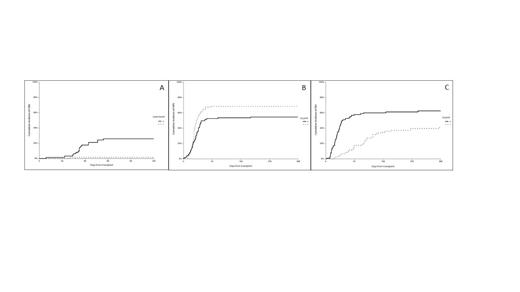
In the group B, reduced intensity conditioning (HR 5.94, p=0.007), letermovir use (HR 0.23, p=0.0009), and aGvHD occurrence (HR 3.13, p=0.007) were independent risk factors for CMV infection in multivariate analysis. The 100-day CI of CMV infection was of 3% (95% CI 1-12) in patients receiving letermovir vs. 26% (95% CI 17-39) in the others (p=0.02, figure 1A). In the same cohort of patients EBV infection appeared to be more frequent for patients receiving ATG (57% vs. 24%, p=0.05), MUD donor (32% vs. 17%, p=0.04) and who experienced CMV concomitant infection (42% vs. 28%, p=0.03). However, these data were not confirmed in multivariate analysis.
According to GvHD prophylaxis, CMV infection appeared to be more frequent in patients receiving Cy-post as GvHD prophylaxis (1-yr CI 68% vs. 54.6%, p=0.02, figure 1B), contrarily to EBV infection which appeared to be less frequent in the same patients (1-yr CI 41% vs. 62%, p<0.0001, figure 1C). However, CMV infection rate was notably reduced by letermovir introduction, while EBV infection rate not appeared to be affected by that.
Figure 1: A) Day 100 cumulative incidence of CMV according to letermovir prophylaxis administration; B) One year cumulative incidence of CMV according to cyclophosphamide post transplant administration; C) One year cumulative incidence of EBV according to cyclophosphamide post transplant administration.
Metafuni: Jazz: Other: Invited Clinical case presentation at meeting. Laurenti: Roche: Honoraria; Gilead: Honoraria; Abbvie: Honoraria, Speakers Bureau; Janssen: Honoraria, Speakers Bureau; AstraZeneca: Honoraria, Speakers Bureau. Sica: Alexion: Consultancy; Jazz Pharma: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal